The Effect of Age on Pancreaticoduodenectomy; Comorbidities, Short-term Outcomes, and Survival
By Umit Ozdemir1, Murat Ulas2, Busra Ekici3, Ahmet Karayigit4, Elif Gundogdu5, Ilter Ozer2Affiliations
doi: 10.29271/jcpsp.2024.03.272ABSTRACT
Objective: To evaluate the complications, mortality, and survival rates of patients aged >70 years undergoing pancreaticoduodenectomy, and to determine associated risk factors.
Study Design: Descriptive study.
Place and Duration of the Study: General Surgery Clinic of Eskişehir Osmangazi University Medical Faculty Hospital, Eskişehir, Turkiye, from January 2014 to September 2020.
Methodology: A retrospective scrutiny of 94 patients who had undergone pancreaticodueodenectomy, was carried out. The patients were separated into two age groups of younger and older than 70 years, and were compared in respect of clinicopathological characteristics, comorbidities, perioperative characteristics, and complications. Independent risk factors for the endpoints of perioperative mortality and survival were investigated.
Results: No significant difference was determined between the groups in respect of biochemical values, and perioperative and histochemical characteristics. Comorbidities were present at a higher rate in the older patients (77.8% vs. 38.8%, p<0.001). The postoperative complication rates were similar (33.3% vs. 32.7%, p=0.944). Perioperative mortality (first 30 days) was determined at a significantly higher rate in the older age group (20.0% vs. 4.1%, p=0.016). The age of patients >70 years increased the risk of mortality 4.851-fold but was not an independent predictive factor (p=0.086). The groups were similar in respect of disease-free survival (DFS) and overall survival (OS, Log-rank p=0.780, p=0.386). Age [Hazard Ratio (HR): 1.029, p=0.048] and pancreas adenocarcinoma (HR: 1.846, p=0.028) were determined to be independent prognostic factors for DFS, and pancreas adenocarcinoma (HR 1.940, p=0.023) for OS.
Conclusion: Older age was not seen to change survival in patients undergoing pancreaticoduodenectomy, but mortality within the first 30 days was affected. Age is not accepted as an absolute contraindication. It is recommended that pancreaticoduodenectomy is performed on patients aged >70 years with careful patient selection, prudent preoperative preparation, a meticulous surgical technique, and close multidisciplinary postoperative support.
Key Words: Pancreaticoduodenectomy, Elderly, Comorbidity, Complication, Mortality, Survival.
INTRODUCTION
As a result of advances in healthcare services and healthcare technology, the mean life expectancy is increasing and there is now a greater proportion of elderly individuals in the total population than in the past.1 The mean life expectancy in Turkiye is 78.6 years for the whole population; 75.9 years for males and 81.3 years for females.2
Although some malignancies reach a peak in a certain age range, the incidence of pancreas adenocarcinoma and other periampullary region tumours increases with increasing age.3 Pancreaticoduodenectomy is accepted as the most complicated abdominal surgical procedure and remains the most effective treatment option since many chemotherapeutic attempts for pancreas head and periampullary region carcinomas have shown disappointing results. With the advances made in surgical techniques and patient care, early mortality rates of pancreaticoduodenectomy have fallen from 30-40% to <5% in high-volume centres.4,5
Together with increasing life expectancy, surgeons now encounter more elderly candidates for pancreaticoduodenectomy. The natural poor prognosis of the disease, the complicated surgical procedure, and the comorbidity status of elderly patients complicate the surgeon’s decision to recommend the surgical option for elderly patients. Conflicting results have been reported of the early morbidity and mortality results and long-term survival of elderly pancreaticoduodenectomy patients in developed regions such as the USA, Western Europe, and Japan. The data from developing countries such as Turkiye, are extremely limited.6-8 The aim of this study was to evaluate the effect of age on the complications, mortality, and survival of patients undergoing pancreaticoduodenectomy.
METHODOLOGY
A retrospective investigation of the data of patients, who underwent pancreaticoduodenectomy in the General Surgery Clinic of Eskişehir Osmangazi University Medical Faculty Hospital between January 2014 and September 2020, was carried out for pancreatic and periampullary region tumours. Patient’s data were retrieved from the hospital database and patient files. All the patients included in the study were aged >18 years and had undergone pancreaticoduodenectomy. The study exclusion criteria were defined as treatment with surgical methods other than pancreaticoduodenectomy, neoadjuvant chemotherapy, R2 resection, or the presence of distant metastasis. As the average life expectancy in Turkiye is 78.6 years, patients aged ≥70 years were compared with patients aged <70 years.2 Approval for the study was granted by the Eskişehir Osmangazi University Medical Faculty Ethics Committee (decision no: 03, dated: 04.05.2021).
For the patients in both age groups, a record of followed parameters was made; age, gender, preoperative biliary stenting (endoscopic retrograde cholangiopancreaticography [ERCP]/percutaneous transhepatic cholangiography [PTC]), preoperative biochemical values (total bilirubin, carbohydrate antigen 19.9 (CA19.9), carcinoembryonic antigen (CEA), albumin), and comorbidities. In addition to the most frequently seen comorbidities of diabetes mellitus (DM), hypertension (HT), and coronary artery disease (CAD), the status of neurological, pulmonary, and vascular comorbidities was also considered. The local tumour depth (T), lymph node metastasis (N), R status, and histological type of malignancy were also included in the evaluations. The postoperative length of stay in hospital, perioperative transfusion requirement, need for reoperation, complications, and costs were examined.
A complication was defined as the emergence of any postoperative surgical or systemic complication. Surgical complications included bleeding, intra-abdominal abscess, and pancreatic fistula (PF). In accordance with the International Study Group of Pancreatic Fistula, PF was defined as drain amylase value 3-fold higher than the serum amylase value after the 3rd postoperative day. Bleeding was accepted as positive in any bleeding situation which needed an intervention or change in treatment. Intraabdominal abscess was defined as the formation of an abscess in the abdomen detected on imaging methods or with reoperation.
The primary endpoint of perioperative mortality (within the first 30 days) and the secondary endpoint of survival status (disease-free survival and overall survival) were compared between the two age groups of patients ≥70 years and <70 years. Independent risk factors were investigated using multivariate analysis.
In all cases, the pancreaticoduodenectomy was performed as previously described by Krausch-Whipple. Hepatoduodenal and paraportal lymph node dissection was performed. The superior mesenteric vein was used as a landmark between the pancreas head and corpus, and the pancreas was divided at this level. When the tumour was seen to continue in the pancreas corpus macroscopically or on frozen section, the pancreatectomy was expanded and cases in which total pancreatectomy was performed were excluded from the study. Pancreaticoenteric anastomosis was made in the form of Cattel-Warren ductojejunostomy, with hepaticoenteric anastomosis and antecholic gastroenteric anastomosis performed on the continuation of the same enteric loop. Postoperative follow-up of the patients included biochemical tests and computed tomography examinations. Adjuvant chemotherapy was recommended by the Oncology Clinic for all the patients.
Data obtained in the study were analysed statistically using SPSS version 25.0 software (SPSS Inc., Chicago, IL, USA). Conformity of numerical variables to normal distribution was examined with visual methods (histogram and probability graphs) and analytical methods (Kolmogorov-Smirnov/ Shapiro-Wilk tests). Descriptive statistics were stated as mean ± standard deviation (SD), or median, minimum-maximum values for continuous variables and as number (n) and percentage (%) for categorical variables. Student’s t-test was applied to data with normal distribution, Mann Whitney U test was used for data not showing normal distribution and Pearson’s Chi-square test was used for categorical data. A value of p<0.05 was accepted as statistically significant.
Univariate and multivariate logistic regression models were used in the determination of risk factors for mortality in the first 30 days postoperatively. Disease-free survival (DFS) and overall survival (OS) were calculated with the Kaplan-Meier method. The Log-Rank test was applied in the analysis of survival curves. Cox regression analysis was used in the determination of independent predictive factors for DFS and OS.
RESULTS
Evaluation was made of a total of 94 patients, separated into two age groups as 49 (52.12%) aged <70 years and 45 (47.87%) aged ≥70 years. The median age of the patients was 64.00 years (range, 37-70 years) in the younger group and 74.00 years (range, 71-84 years) in the older group.
The patient characteristics and comorbidities are presented in Table I. Gender distribution was similar in both age groups. No significant difference was determined between the groups in respect of preoperative biliary stenting (ERCP/PTC) or preoperative biochemical values (CA19.9, CEA, albumin, total bilirubin). Comorbidities were significantly more common in the older patients (≥70 years, p<0.001).
Table I: Patients’ characteristics, comorbidities and perioperative data, complications and mortality.
|
|
≤70 Age n: 49 (52.12%) |
>70 Age n: 45 (47.87%) |
p-value* |
|
Ageᵃ |
64,00 (37 – 70) |
74 (71 – 84) |
|
|
Gender (male) |
|
|
0,558 |
|
Male |
28 (57.1 %) |
23 (51.1 %) |
|
|
Female |
21 (42.9 %) |
22 (48.9 %) |
|
|
Comorbidity |
|
|
<0.001 |
|
Present |
19 (38.8 %) |
35 (77,8 %) |
|
|
Not present |
30 (61.2 %) |
10 (22.2 %) |
|
|
2 and more comorbidities |
|
|
0.024 |
|
2 and more |
12 (24,5 %) |
21 (46.7 %) |
|
|
0 or 1 comorbidity |
37 (75.5 %) |
24 (53.3 %) |
|
|
DMᵇ |
8 (16.3 %) |
16 (35.6 %) |
0.033 |
|
HTᵇ |
18 (36.7 %) |
23 (51.1 %) |
0.160 |
|
Coronary artery diseasesᵇ |
6 (12.2 %) |
6 (13.3 %) |
0.874 |
|
Neurologic comorbitiesᵇ |
1 (2.0 %) |
2 (4.4 %) |
0.605 |
|
Pulmoner comorbitiesᵇ |
2 (4.1 %) |
3 (6.7 %) |
0.668 |
|
Vascular comorbitiesᵇ |
0 (0.0 %) |
2 (4,4 %) |
0.226 |
|
Preoperative biliary stenting (ercp/ptc) |
25 (51.0 %) |
25 (55.6 %) |
0.660 |
|
Preoperative Total bilirubinᵃ |
3.19 (0,14 – 23.13) |
2.32 (0.09 – 26.9) |
0.961 |
|
Preoperative CA 19.9ᵃ |
82.58 (0.20 – 10000.0) |
103.0 (0.20 – 4505) |
0.464 |
|
Preoperative CEAᵃ |
3.18 (0.60 – 25.2) |
3.83 (1.18 – 914.0) |
0.428 |
|
Length of stayᵃ |
13 (3 – 38) |
14,5 (2 – 45) |
0.202 |
|
Costᶜ |
21015.29 ± 8023.58 |
23051.36 ±8753.19 |
0.242 (-5472.64 to 1400.50)ᵈ |
|
Perioperative Transfusionᵇ |
21 (42.9 %) |
26 (57.8 %) |
0.148 |
|
reoperationᵇ |
5 (10.2 %) |
2 (%4.4) |
0.438 |
|
Complicationᵇ |
16 (32.7 %) |
15 (33.3 %) |
0.944 |
|
Bleedingᵇ |
2 (4.1 %) |
2 (4.4 %) |
>0.99 |
|
İntraabdominal abscessᵇ |
4 (8.2 %) |
3 (6.7 %) |
>0.99 |
|
Pancreatic fistulaᵇ |
9 (28.1 %) |
11 (42.3 %) |
0.258 |
|
T3-4ᵇ |
18 (36.7 %) |
11 (25.0 %) |
0.223 |
|
N+ᵇ |
41 (83.7 %) |
24 (53.3 %) |
0.001 |
|
R1ᵇ |
15 (31.3 %) |
10 (22.7 %) |
0.359 |
|
Pancreas Adenocarsinomaᵇ |
30 (61.2 %) |
28 (62.2 %) |
0.921 |
|
First 30-day mortality |
|
|
0.016 |
|
Present |
2 (4.1 %) |
9 (20.0 %) |
|
|
Not present |
47 (95.9 %) |
36 (80.0 %) |
|
|
ᵃMedian (min-max), ᵇPresent ᶜMean ± standard deviation, ᵈ95% confidence interval of difference, *Mann Whitney U test, Pearson’s Chi-square test, independent samples t-test. |
|||
Table II: predictive factors of first 30 days mortality, univariate and multivariate logistic regression analysis.
|
|
Univariate p |
Multivariate p |
Odds ratio |
95% CI for Odds ratio |
|
Age |
0.029 |
0.086 |
4.851 |
0.800 to 29.39 |
|
Gender |
0.535 |
|
|
|
|
Comorbidity |
0.284 |
0.826 |
1.202 |
0.233 to 6.195 |
|
Preoperative total bilirubin |
0.495 |
|
|
|
|
CA 19.9 |
0.998 |
|
|
|
|
Transfusion |
0.749 |
|
|
|
|
Complication |
0.116 |
0.112 |
3.0.80 |
0.769 to 12.33 |
|
Reoperation |
0.825 |
|
|
|
|
R status |
0.480 |
|
|
|
|
T3-4 status |
0.126 |
0.212 |
0.247 |
0.028 to 2.219 |
|
N status |
0.081 |
0.335 |
0.497 |
0.120 to 2.060 |
|
Pancreas Adenocarcinoma |
0.604 |
|
|
|
Table III: Cox regression analysis for disesae-free survival and overall survival.
|
|
For DFS |
For OS |
|||||
|
HR |
95% CI for HR |
p |
HR |
95% CI for HR |
p |
||
|
Age |
1.029 |
1.000 to 1.059 |
0.048 |
1.025 |
0.993 to 1.058 |
0.123 |
|
|
Comorbidity |
0.724 |
0.416 to 1.260 |
0.254 |
0.930 |
0.521 to 1.660 |
0.806 |
|
|
Complication |
0.943 |
0.533 to 1.668 |
0.839 |
0.964 |
0.525 to 1.773 |
0.907 |
|
|
R status |
0.983 |
0.555 to 1.740 |
0.952 |
1.060 |
0.586 to 1.916 |
0.848 |
|
|
Pancreas CA |
1.846 |
1.069 to 3.187 |
0.028 |
1.940 |
1.096 to 3.431 |
0.023 |
|
When the status of having 2 or more comorbidities was examined, the rate was higher in the older age group (p=0.024). Of the preoperative comorbidities, DM was seen significantly more in the older age group (p=0.033), and HT was more frequent in the older patients but not to a level of statistical significance (51.1% vs.36.7%, p=0.160). The distribution of CAD, neurological comorbidities, pulmonary comorbidities, and vascular comorbidities was similar in both age groups (Table I).
The perioperative data, complications, and mortality rates are presented in Table I. The length of stay in hospital, costs, and re-operation rates were similar in the two groups. There was a greater tendency for perioperative erythrocyte transfusion in the older patient group than in the younger (57.8% vs.42.9%, p=0.148). Complications developed at similar rates in both groups. The distribution of surgical complications such as bleeding, pancreatic fistula, and intra-abdominal abscess was similar between the groups, and there was no difference in respect of tumour local depth (T), type of malignancy (pancreatic adenocarcinoma vs. others) and R status. In the histochemical analysis, the rate of lymph node positivity (N+) was determined to be higher in the younger patient group compared to the older group (83.7% vs. 53.3%, p=0.001, Table I).
Perioperative mortality, defined as within the first 30 days, occurred more often in the older patients than in the younger group (20.0% vs. 4.1%, p=0.016, Table I). A logistic regression model was formed to investigate the risk factors of 30-day mortality (Table II). The results of the multivariate analysis showed that lymph node positivity(N+), local depth of the tumour (T3-4), the presence of comorbidities, and the development of postoperative complications were not evaluated as independent risk factors for 30-day mortality. Older age increased the risk 4.851-fold (odds ratio)but was not determined to be an independent predictive factor (p=0.086, Table II).
The mean follow-up period of all the patients was median 14.00 months (range, 1.00-85.00 months). In the older patient group aged ≥70 years, the 1-year DFS rate was 46.6%, 3-year DFS was 26.7%, and mean DFS was 23.6 months (95% CI:14.03-32.09). In the younger patient group aged <70 years, the 1-year DFS rate was 61.8%, 3-year DFS was 13.0%, and mean DFS was 22.79 months (95% CI:14.47-31.12). The groups were determined to be similar in respect of DFS (Log-rank p=0.780, Figure 1). In the older patient group aged ≥70 years, the 1-year OS rate was 48.9%, 3-year OS was 34.4%, and mean OS was 24.89 months (95% CI:15.16-34.62). In the younger patient group aged <70 years, the 1-year OS rate was 76.7%, 3-year OS was 16.8%, and mean OS was 27.27 months (95% CI:18.93-35.61). Age was not determined to have affected overall survival (Log-rank p=0.386, Figure 2).
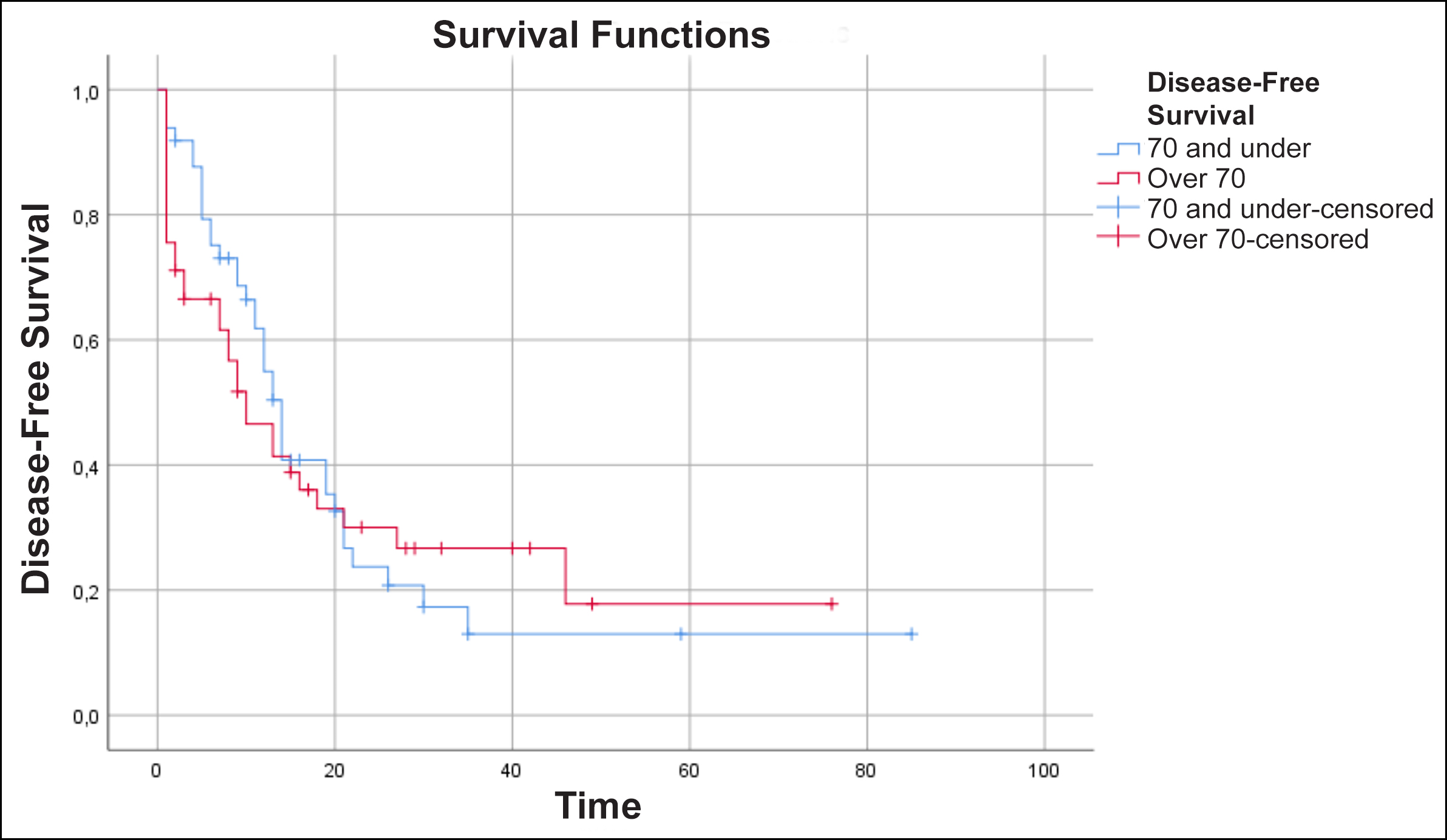 Figure 1: Disease-free survival Kaplan meier curve, log rank p=0.780.
Figure 1: Disease-free survival Kaplan meier curve, log rank p=0.780.
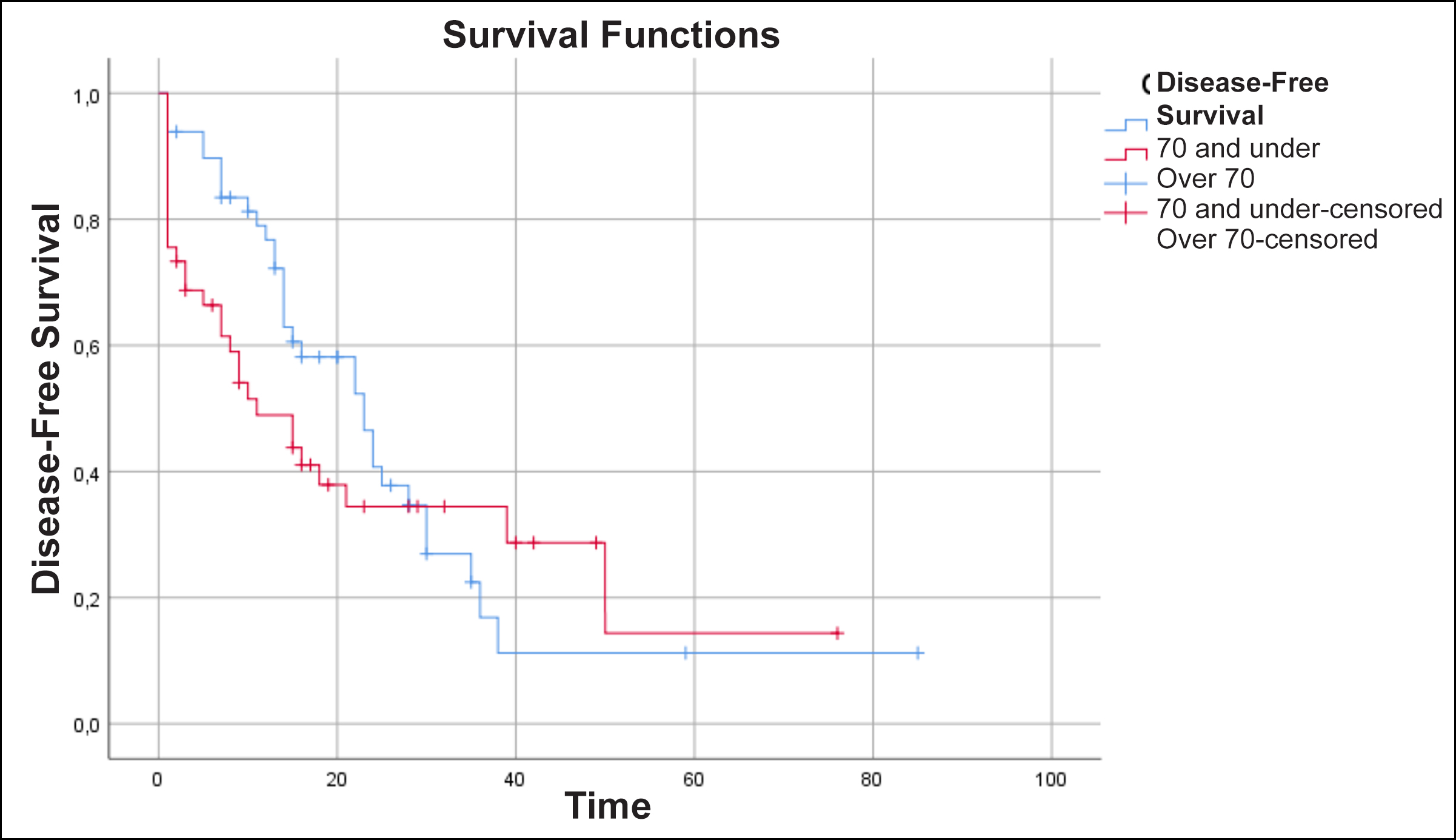 Figure 2: Overall survival Kaplan meier curve, log rank p=0.386.
Figure 2: Overall survival Kaplan meier curve, log rank p=0.386.
A Cox regression model was applied for the evaluation of prognostic factors affecting survival. The results showed that age (Hazard Ratio (HR): 1.029, 95% CI for HR: 1.000 - 1.059, p=0.048) and malignancy type of pancreas adenocarcinoma (HR: 1.846, 95% CI for HR: 1.069 to 3.187, p=0.028) were independent prognostic factors for DFS. For OS, only malignancy type of pancreas adenocarcinoma was determined to be an independent prognostic factor (HR:1.940, 95% CI for HR: 1.096 - 3.431, p=0.023). Preoperative comorbidities, postoperative complications, and R status were not found to affect survival (Table III).
DISCUSSION
Together with ongoing developments in healthcare knowledge and technology, the global elderly population is also increasing. With the increase in average life expectancy, there has also been an increase in the age of diagnosis of pancreatic and periampullary region malignancies, for which curative treatment is possible with surgery.9 However, despite significant developments in surgical technique, pancreaticoduodenectomy remains a complicated surgical intervention with severe difficulties in postoperative care. Therefore, there continues to be debate in literature on the subject of pancreaticoduodenectomy in elderly patients who have increased comorbidities and decreased performance.10 In various studies, there are even different cut-off points for the definition of “older patient”.11,12 Taking the starting point of average life expectancy in Turkiye of 78.6 years, the cut-off value for the age groups in the current study was defined as 70 years.2
The results of this study showed that comorbidities were seen at a higher rate in the older patient group (≥70 years, 38.3% vs.78.8%, p<0.001). When the comorbidities were examined separately, DM was determined at a higher rate in the older patient group. There is generally an increase in comorbidities with advancing age, and therefore comorbidities or mortality may increase.7,12,13 However, in the current study, comorbidities were not seen to show an independent effect on 30-day mortality or survival. The reason for this was thought to be that in recent decades advances have been made in patient care and the treatment of chronic diseases with the developments in medical knowledge and technology. The two age groups in the current study were seen to be similar in respect of preoperative biliary stenting, CEA and CA19.9 values showing the tumour burden, and albumin values providing information about the nutritional status. These parameters were similar in the two groups allowed a clearer evaluation of the effect of age on the primary endpoints of 30-day mortality and survival, independently of other factors.
The complication rates were similar in the older (≥70 years) and younger (<70 years) patient groups in the current study. Although there are studies in literature stating that older patients tend to have more complications, the general view is that age does not make a difference, consistent with the current study results.7,8,14,15 Again consistent with previous studies, the length of hospital stay was similar in the current study groups.6,7,16 Very few studies in literature have mentioned costs, and the basic factors affecting costs are length of hospital stay and complications.17,18 As the current study groups were similar for the reasons stated above, there was no difference in respect of costs. Preventative measures for elderly patients such as age-related care, supplemental enteral nutrition, and early rehabilitation placement are important to avoid complications and thereby avoid increased costs.19 The rates of pancreatic adenocarcinoma were similar in the two groups in the current study but lymph node involvement was determined at a higher rate in the younger group. It was thought that this may have been due to more aggressive surgery having been performed encouraged by the fact of younger age and fewer comorbidities.
In previous studies, 30-day mortality has been shown to be 0-8% in groups aged > 70 years and 0-17% in those aged <70 years.7 In the current study, this rate was calculated as 4.1% in the <70 years age group and 20.0% in the >70 years age group (p=0.016). However, in the multivariate analysis, age was not evaluated as an independent risk factor for 30-day mortality (p=0.086). On the subject of first 30-day mortality or in-hospital mortality, it is a fact that there is a greater tendency for mortality in the elderly.8,11 Although some studies have shown that age makes no significant difference to 30-day mortality, many studies have reported that despite greater elderly mortality, a significant increase has not been determined.6,7,10,14,20,21 The heterogeneity that has emerged in other studies was also seen in this study. Age was determined to be significant in mortality but was not an independent risk factor. There are insufficient satisfactory data in the current and previous studies to justify avoiding pancreaticoduodenectomy in elderly patients in respect of early mortality.
In the available literature, overall survival has been reported as 16-24 months for the <70 years age group and 9-19.8 months for those aged >70 years.7,8,12 In the majority of studies, age has been shown to have no effect on survival.22-24 Similarly in the current study, there was seen to be no difference between the groups in respect of DFS and OS. The 1-year DFS and OS rates were higher in the younger group, while the 3-year survival rates were higher in the older group. The reason for this could have been that although there is no change in tumour biology with age, the low performance and nutritional status, especially in those with severe comorbid failures, could have caused bias in the selection of elderly patients.
In parallel with the literature, pancreas adenocarcinoma was evaluated as an independent prognostic factor in the multivariate analysis of OS and DFS.25 While age was an independent prognostic factor for DFS, it was not for OS. Age is not a barrier to pancreaticoduodenectomy in respect of survival, and elderly patients deserve meticulous surgery. The heterogeneous results that emerged from the investigation of prognostic factors for DFS and OS show the need for further more comprehensive research with homogenous and larger patient series.
There were some limitations to this study, primarily the retrospective design, and the relatively low number of patients, but the group numbers were balanced at 45 and 49. Another limitation could be said to be that when potential patients for pancreaticoduodenectomy present to a surgeon, the surgeon may not be willing to perform resection in some elderly patients for reasons such as the performance and nutritional status of the patient, severe systemic failures, and restricted mobilisation, and this could have created a selection bias. However, the higher rate of comorbidities in the older patient group in this study was reflected in the statistical results, so there can be considered to have been no or relatively limited selection bias.
CONCLUSION
The results of this study demonstrated that despite the higher rates of comorbidities in older patients (>70 years), this did not increase the complication rates in pancreaticoduodenectomy. When it is considered that pancreaticoduodenectomy makes a great contribution to survival and is the only curative option, it can be recommended that with careful patient selection, prudent preoperative preparation, a meticulous surgical technique, and close multidisciplinary postoperative support, pancreaticoduodenectomy can be performed on elderly patients as survival does not alter with increasing age although the first 30-day mortality is affected.
ETHICAL APPROVAL:
Approval for the study was granted by the Eskişehir Osmangazi University Medical Faculty Ethics Committee (decision no: 03, dated: 04.05.2021).
PATIENTS’ CONSENT:
Due to the descriptive, retrospective nature of the study, patient’s consent was not obtained.
COMPETING INTEREST:
There was no conflict of interest declared by the authors.
AUTHORS’ CONTRIBUTION:
UO: Conceptualisation, methodology, formal analysis and investigation, drafting, review and editing, esources.
MU, IO: Conceptualisation, supervision.
BE: Formal analysis and investigation, drafting, esources.
AK: Methodology, drafting, review, and editing.
EG: Conceptualisation, formal analysis and investigation, esources.
REFERENCES
- Etzioni DA, Liu JH, Maggard MA, Ko CY. The aging population and its impact on the surgery workforce. Ann Surg 2003; 238(2):170-7. doi: 10.1097/01.SLA.0000081085.98792.3d.
- Turkiye İstatistik Kurumu (Turkish Statistical Institute). Hayat Tabloları (Life Tables) 2017-2019 [Available from: https://data.tuik.gov.tr/Bulten/Index?p=Hayat-Tablolari-2017-2019-33711. cited 27 January 2024).
- Riall TS. What is the effect of age on pancreatic resection? Adv Surg 2009; 43(1):233-49. doi: 10.1016/j.yasu.2009. 02.004.
- Ho V, Heslin MJ, Effect of hospital volume and experience on in-hospital mortality for pancreaticoduodenectomy. Ann surg 2003; 237(4):509. doi: 10.1097/01.SLA.00000599 81.13160.97
- Jamal A, Shakeel O, Mohsin J, Malik AA, Haq IU, Begum S, et al. Pancreaticoduodenectomy: Outcomes of a complex surgical procedure from a developing country. Pancreatology 2020; 20(7):1534-9. doi: 10.1016/j.pan.2020.08.013.
- Adham M, Bredt LC, Robert M, Perinel J, Lombard-Bohas C, Ponchon T, et al. Pancreatic resection in elderly patients: Should it be denied? Langenbecks Arch Surg 2014; 399: 449-59. doi: 10.1007/s00423-014-1183-9.
- Miyazaki Y, Kokudo T, Amikura K, Kageyama Y, Takahashi A, Ohkohchi N, et al. Age does not affect complications and overall survival rate after pancreaticoduodenectomy: single-center experience and systematic review of literature. Biosci Trends 2016; 10(4):300-6. doi: 10.5582/bst.2016. 01093.
- De Franco V, Frampas E, Wong M, Meurette G, Charvin M, Leborgne J, et al. Safety and feasibility of pancreaticoduodenectomy in the elderly: A matched study. Pancreas 2011; 40(6):920-4. doi: 10.1097/MPA.0b013e31821fd70b.
- Sukharamwala P, Thoens J, Szuchmacher M, Smith J, DeVito P. Advanced age is a risk factor for post-operative complications and mortality after a pancreaticoduodenectomy: a meta-analysis and systematic review. HBP Oxford 2012; 14:877. doi: 10.1111/j.1477-2574.2012.00506.x.
- Riall TS, Reddy DM, Nealon WH, Goodwin JS. The effect of age on short-term outcomes after pancreatic resection: A population-based study. Ann Surg 2008; 248(3):459. doi: 10.1097/SLA.0b013e318185e1b3.
- Zhang W, Huang Z, Zhang J, Che X. Safety and effectiveness of open pancreaticoduodenectomy in adults aged 70 or older: A meta-analysis. J Geriatr Oncol 2021; 12(7): 1136-45. doi: 10.1016/j.jgo.2021.02.004.
- Renz BW, Khalil PN, Mikhailov M, Graf S, Schiergens TS, Niess H, et al. Pancreaticoduodenectomy for adenocarcinoma of the pancreatic head is justified in elderly patients: A retrospective cohort study. Int J Surg 2016; 28:118-25. doi: 10.1016/j.ijsu.2016.02.064.
- Casadei R, Taffurelli G, Silvestri S, Ricci C, Campra D, Minni F. et al. Is age a barrier to pancreaticoduodenectomy? An Italian dual-institution study. Updates Surg 2015; 67: 439-47. doi: 10.1007/s13304-015-0337-9.
- Urbonas K, Gulbinas A, Smailyte G, Pranys D, Jakstaite A, Pundzius J, et al. Factors influencing survival after pancreatoduodenectomy for ductal adenocarcinoma depend on patients' age. Dig Surg 2015; 32(1):60-7. doi: 10.1159/000 371856.
- Usuba T, Takeda Y, Murakami K, Tanaka Y, Hanyu N. Clinical outcomes after pancreaticoduodenectomy in elderly patients at middle-volume center. Hepatogastroenterology 2014; 61(134):1762-6.
- El Nakeeb A, Atef E, El Hanafy E, Salem A, Askar W, Ezzat H, et al. Outcomes of pancreaticoduodenectomy in elderly patients. Hepatobiliary Pancreat Dis Int 2016; 15(4):419-27. doi: 10.1016/S1499-3872(16)60105-4.
- Vickers SM, Kerby JD, Smoot TM, Shumate CR, Halpern NB, Aldrete JS, et al. Economics of pancreatoduodenectomy in the elderly. Surgery 1996; 120(4):620-6. doi: 10.1016/S00 39-6060(96)80008-0.
- Topal B, Peeters G, Vandeweyei H, Aerts R, Penninckx F. Hospital cost-categories of pancreaticoduodenectomy. Acta Chir Belg 2007; 107(4):373-7. doi: 10.1080/00015 458. 2007.11680078.
- Pratt WB, Gangavati A, Agarwal K, Schreiber R, Lipsitz LA, Callery MP, et al. Establishing standards of quality for elderly patients undergoing pancreatic resection. Arch Surg 2009; 144(10):950-6. doi: 10.1001/archsurg.2009.107.
- Kimura W, Miyata H, Gotoh M, Hirai I, Kenjo A, Kitagawa Y, et al. A pancreaticoduodenectomy risk model derived from 8575 cases from a national single-race population (Japanese) using a web-based data entry system: the 30-day and in-hospital mortality rates for pancreaticoduodenectomy. Ann Surg 2014; 259(4):773-80. doi: 10.1097/SLA.00000000 00000263.
- Pedziwiatr M, Małczak P, Mizera M, Witowski J, Torbicz G, Major P, et al. Pancreatoduodenectomy for pancreatic head tumors in the elderly–systematic review and meta-analysis. Surg Oncol 2018; 27(3):346-64. doi: 10.1016/j.suronc. 2018.05.021.
- Bathe OF, Levi D, Caldera H, Franceschi D, Raez L, Patel A, et al. Radical resection of periampullary tumors in the elderly: evaluation of long-term results. World J Surg 2000; 24(3):353-8. doi: 10.1007/s002689910056.
- Di Carlo V, Balzano G, Zerbi A, Villa E. Pancreatic cancer resection in elderly patients. BJS 1998; 85(5):607-10. doi: 10.1046/j.1365-2168.1998.00685.x.
- Fong Y, Blumgart LH, Fortner JG, Brennan MF. Pancreatic or liver resection for malignancy is safe and effective for the elderly. Ann Surg 1995; 222(4):426. doi: 10.1097/000 00658-199522240-00002.
- Lee MK, DiNorcia J, Reavey PL, Holden MM, Genkinger JM, Lee JA, et al. Pancreaticoduodenectomy can be performed safely in patients aged 80 years and older. J Gastrointest Surg 2010; 14(11):1838-46. doi: 10.1007/s11605-010-13 45-1.